Thousands of Kentucky’s Newly Insured Turn to KVC

The Affordable Care Act has increased the number of low-income people who can access behavioral healthcare for problems such as depression, anxiety, thoughts of self-harm, the effects of childhood traumatic stress, and substance abuse disorders.
The Commonwealth of Kentucky has been leading the charge to implement healthcare reform, including expanding Medicaid services. Gov. Steve Beshear supported the creation of the state’s health benefit exchange, Kynect, which has enrolled more than half a million Kentuckians. Three-fourths of those who enrolled had no health insurance previously. These changes mean that the state has successfully created the nation’s second largest reduction in the percentage of uninsured people–from 20.4% to just 11.9%.
Since the majority of Kentucky’s newly insured are on Medicaid, this shift created a problem–increased ‘demand’ for behavioral health services clashed with an inadequate ‘supply’ of qualified providers. This unbalanced behavioral healthcare market existed, in part, because for decades only community mental health centers could serve Medicaid clients, except for special contracts. IMPACT Plus was one of those special contracts that allowed KVC Kentucky to provide a limited level of services to children, but this new model caught the attention of Kentucky’s policymakers.
To more effectively meet the needs of the newly insured, the state has changed the old rules so that now ‘any willing provider’ of mental health services can serve Medicaid clients. This has opened the door for Kentuckians to receive enhanced support from KVC Kentucky.
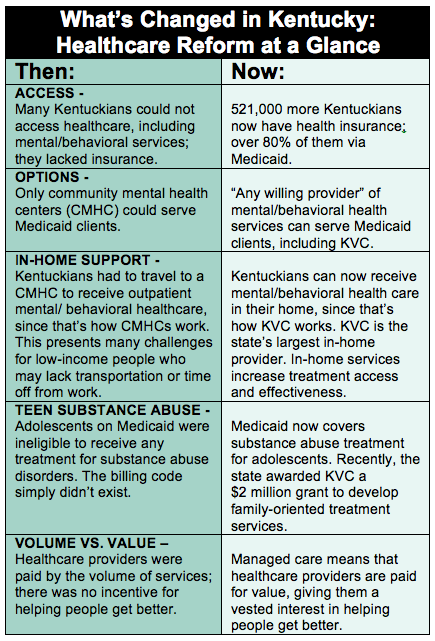 This change doesn’t mean that instead of driving to a community mental health center for treatment, clients now drive to a KVC office. Instead, it means that a highly skilled, caring KVC therapist can come into their home to provide treatment. KVC is the largest provider of in-home services in the state. Providing mental and behavioral healthcare in the home not only makes treatment more accessible, but research shows that it also makes it more effective than therapy in traditional outpatient settings. In addition, clients are no longer required to “fail” in traditional outpatient therapy to qualify for in-home therapy—they can be directed into this more intensive form of intervention based on a valid assessment that they would benefit.
This change doesn’t mean that instead of driving to a community mental health center for treatment, clients now drive to a KVC office. Instead, it means that a highly skilled, caring KVC therapist can come into their home to provide treatment. KVC is the largest provider of in-home services in the state. Providing mental and behavioral healthcare in the home not only makes treatment more accessible, but research shows that it also makes it more effective than therapy in traditional outpatient settings. In addition, clients are no longer required to “fail” in traditional outpatient therapy to qualify for in-home therapy—they can be directed into this more intensive form of intervention based on a valid assessment that they would benefit.
Another major change is in the area of substance abuse treatment. In the past, there were no services available for an adolescent on Medicaid who might be struggling with a drug or alcohol addiction, such as youth in foster care or in low-income families. There literally was no billing code, and thus no way for any provider to get paid for providing these crucial services.
That changed recently with the KY Kids Recovery Program, which is underwritten by funds generated by a legal settlement between the state and two pharmaceutical companies. Gov. and Mrs. Beshear, along with KY Attorney General Jack Conway and members of the Substance Abuse Treatment Advisory Committee, directed $20 million of the $32 million settlement to expand substance abuse treatment, including opiate addiction services.
The state recently awarded KVC the largest KY Kids Recovery Program grant to date – over $2 million – for the large-scale implementation of evidence-based, in-home services to treat adolescents with substance abuse and co-occurring disorders across 59 counties in central and eastern Kentucky.
While healthcare reform is driving major changes for KVC Kentucky as an organization, these changes are even more significant in the lives of children and families.

Elizabeth Croney, President of KVC Kentucky
“Previously, the IMPACT Plus program only allowed us to provide behavioral health care to children, and the maximum treatment period was six months,” said Elizabeth Croney, President of KVC Kentucky. “Once that child met their initial treatment goals, they couldn’t continue with us. A child may have still needed therapy once a week or booster-sessions six or 12 months down the road, but the old rules meant they’d have to start all over again with another organization—a real disincentive for families to maintain their child’s progress. Furthermore, we weren’t able to treat parents, yet often we found that a parent struggling with depression and other mental health issues was negatively affecting the child’s recovery process.”
That’s all changed in the last year. “Now we can integrate KVC services in such a way that our families will experience the important gains that come with continuation of care,” continued Croney. “The fact that KVC can now serve children and adults alike and that treatment can be sustained as needed beyond the arbitrary six month limit is positively changing everything.”
Those rule changes, along with KVC’s unique in-home service delivery model, mean that the people of Kentucky now have ready access to local behavioral health care providers who use research-backed approaches that are proven to work.
“For years we have demonstrated that our model works with children, and we want to expand the model to help adults… KVC’s approach is making a real difference in people’s lives.” – Elizabeth Croney, President of KVC Kentucky
“We’ve always been the largest in-home service provider in Kentucky,” said Croney. “For years we have demonstrated that our model works with children, and we want to expand the model to help adults. KVC has achieved a 93% diversion rate, which means our intensive in-home services are helping children stay safely at home rather than going into foster care. We’re helping clients get better and to ‘step down’ into a less intrusive and less costly level of care. KVC’s approach is making a real difference in people’s lives.”
Clients who are covered by CoventyCares of Kentucky/Aetna, Blue Cross Blue Shield and Humana are all now eligible to receive services from KVC Kentucky. Visit kentucky.kvc.org to learn more.